Going to the doctor shouldn’t feel like a risk. But for many sex workers, stepping into a clinic means walking into a room where judgment is louder than the nurse’s greeting. You’re not just there for a checkup-you’re there hoping not to be shamed, ignored, or refused care because of what you do for a living. This isn’t rare. It’s everyday.
What Happens When You Walk Into a Clinic
Imagine you’re dealing with a persistent sore throat, a strange rash, or unexplained bleeding. You’ve tried home remedies. You’ve waited too long. You finally make the appointment. You tell the receptionist you’re here for a general checkup. When the doctor walks in, you hesitate. Do you say it? Do you say, I’m a sex worker? If you do, the response might be silence. Or worse-a shift in tone. A raised eyebrow. A quick change in the script: “Let’s test for STIs,” as if that’s the only thing you could possibly need. Or worse: “You should really consider a different line of work.” A 2024 study by the Global Network of Sex Work Projects found that 68% of sex workers in high-income countries reported being refused care or treated disrespectfully by healthcare providers in the past year. In Australia, where sex work is decriminalized in some states but still heavily stigmatized, the problem is just as real. Nurses have walked out of rooms. Doctors have refused to perform Pap smears. Clinics have asked sex workers to reschedule “because of the nature of your work.” This isn’t about health. It’s about bias. And bias kills.Why Stigma Is a Public Health Crisis
When people avoid care because they fear being judged, the consequences aren’t just personal-they ripple outward. Sex workers are more likely to delay testing for HIV, hepatitis, or chlamydia. They skip vaccinations. They don’t get regular cervical screenings. They avoid mental health support because therapy feels like another place they’ll be labeled “high-risk” instead of “in need of help.” The World Health Organization says stigma is one of the top barriers to effective HIV prevention. And yet, most health systems still treat sex workers as a problem to manage-not people to serve. The result? Higher rates of preventable infections. Longer hospital stays. More deaths. In Perth, where decriminalization has been in place since 1994, sex workers still report being turned away from public hospitals during emergencies. One woman, who asked to remain anonymous, went to the ER after a violent assault. The triage nurse asked if she was “working that night.” When she said yes, the nurse said, “We’ll call the police.” She left without treatment. This isn’t healthcare. It’s punishment by proxy.What Safe Healthcare Actually Looks Like
Safe healthcare for sex workers doesn’t require fancy equipment or expensive drugs. It requires three things: respect, training, and choice. First, respect. That means not assuming your health needs are only sexual. A sex worker can have a broken wrist, diabetes, depression, or a migraine. Your job doesn’t define your body. Second, training. Medical staff need to understand the realities of sex work-not from moral panic, but from evidence. They need to know that decriminalization improves health outcomes. That peer-led outreach works. That trauma-informed care isn’t a buzzword-it’s a necessity. Third, choice. You should be able to choose who you see. Some sex workers prefer clinics that specialize in sex worker health. Others want to go to their local GP. Both should be options. No one should be funneled into a “sex worker clinic” like it’s a separate caste system. In Melbourne, the Sex Workers Outreach Project runs a free clinic staffed by nurses who’ve worked with sex workers for over a decade. No forms asking for your “occupation.” No judgment. Just blood tests, condoms, PrEP, and a cup of tea. That’s what healthcare should be.
How to Find a Safe Provider
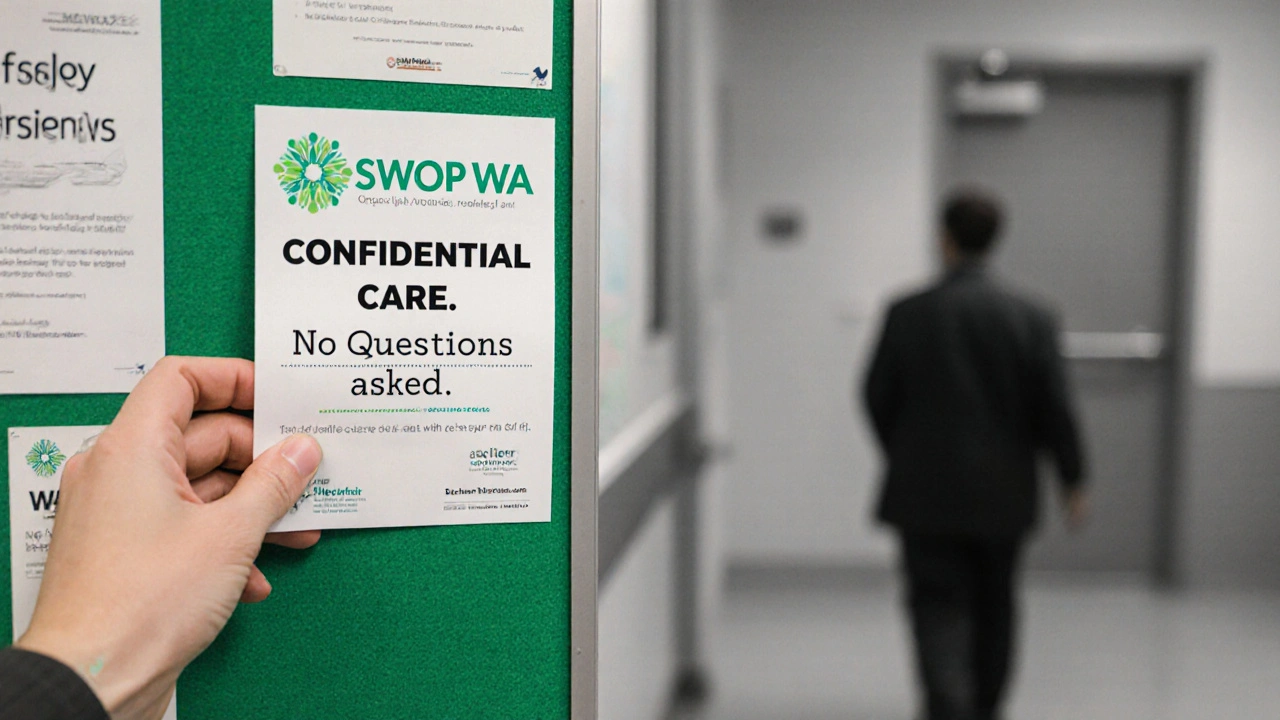
You don’t have to suffer in silence. Here’s how to find care that doesn’t make you feel like a criminal:- Look for clinics affiliated with sex worker-led organizations. In Australia, groups like SWOP WA (Perth), SWOP NSW, and Scarlet Alliance have partnerships with doctors who understand your needs.
- Call ahead. Ask: “Do you have experience working with sex workers? Do you offer confidential STI testing without reporting?” If they hesitate, move on.
- Use peer networks. Many sex workers share lists of safe providers through encrypted apps or community groups. Ask someone you trust.
- Bring a friend. Having someone with you can reduce pressure and help you remember questions.
- Know your rights. In Western Australia, you have the right to refuse to disclose your occupation. No provider can legally force you to say what you do.
What to Say (and Not Say) at Your Appointment
You don’t owe anyone your life story. But if you want to get the care you need, here’s how to navigate the conversation:- Start simple: “I’m here for a checkup. I’m concerned about [symptom].”
- If they ask about your job, you can say: “I’d prefer not to discuss my occupation. Can we focus on my health?”
- If they press: “I’m not comfortable answering that. I’m here for medical care, not a moral evaluation.”
- If they refuse care: “I’m filing a complaint with the health ombudsman. Is there another provider I can see today?”
When the System Fails You
Sometimes, even after you’ve done everything right, the system still lets you down. You get turned away. You’re gaslit. You’re told your symptoms are “all in your head.” Here’s what to do:- Document everything. Write down the date, time, name of the provider, and what was said. Even if you’re upset, write it down. Later, you can file a formal complaint.
- Report to the Health and Disability Commissioner (in WA) or your state’s equivalent. They can investigate discrimination.
- Reach out to advocacy groups. Scarlet Alliance and SWOP WA can help you file complaints, connect you with legal aid, or even arrange a new appointment.
- Don’t blame yourself. This isn’t your fault. The system failed you-not you failing the system.
Change Is Possible-And It’s Already Happening
In 2023, the Royal Australian College of General Practitioners updated its guidelines to include mandatory training on stigma reduction for all registered GPs. That’s a big step. It doesn’t fix everything, but it’s a start. In Sydney, a pilot program trained 80 doctors in trauma-informed care for sex workers. Within a year, clinic attendance among sex workers rose by 42%. STI detection rates went up-not because people were riskier, but because they felt safe enough to show up. This isn’t about special treatment. It’s about equal treatment.You Deserve Care
You are not your job. You are not a statistic. You are not a risk factor. You are a person with a body that needs care-just like everyone else. The healthcare system should meet you where you are. Not where they think you should be. If you’ve been turned away, you’re not alone. If you’re scared to go back, that’s understandable. But you don’t have to keep suffering in silence. There are people who will listen. There are clinics that will help. And there’s a growing movement that says: your health matters. Your life isn’t a crime. Your body isn’t a violation. And your right to care? That’s not up for debate.Can I be forced to disclose that I’m a sex worker at a clinic?
No. In Australia, you have the legal right to refuse to disclose your occupation. Healthcare providers cannot require you to reveal your job, and refusing to answer does not justify denying you care. If a provider pressures you, you can report them to your state’s health ombudsman.
Are there clinics in Perth that specialize in sex worker health?
Yes. SWOP WA (Sex Workers Outreach Project Western Australia) partners with several clinics in Perth that offer confidential, stigma-free care. They provide free STI testing, PrEP access, vaccinations, and mental health referrals. You don’t need an appointment-drop-ins are welcome. Their staff are trained by sex workers themselves.
Can I get PrEP without being judged?
Absolutely. PrEP is available through general practitioners, sexual health clinics, and community health centers across Australia. Many providers now offer it without asking about your job. If you’re turned away, ask for another doctor or contact Scarlet Alliance-they can connect you with a provider who won’t make you feel ashamed.
What if I’m undocumented or on a visa?
In Australia, you can access free STI testing and emergency care regardless of visa status. Public hospitals cannot deny emergency treatment. For non-emergency care, some clinics offer sliding scale fees or free services through community health programs. Contact SWOP WA or local refugee health services-they help people of all immigration statuses.
How do I know if a provider is truly safe?
Look for clinics that partner with sex worker organizations. Ask if staff have received training from groups like SWOP or Scarlet Alliance. If they use terms like “high-risk” or “prostitution,” that’s a red flag. Safe providers say “sex worker,” not “prostitute.” They don’t assume your health needs. They listen. And they never make you feel like a burden.
